Niger J Paed 2016; 43 (1): 34-39
ORIGINAL
Musa S
Prevalence of hepatitis C Antibody
Yakubu AM
in Human Immunodeficiency Virus
Muktar HM
infected children
DOI:http://dx.doi.org/10.4314/njp.v43i1.7
Accepted: 25th October 2015
Abstract :
Background: Hepatitis
both subjects (92.3%) and controls
C
virus (HCV) is a major public
(100.0%). Injection at patent medi-
Musa S
(
)
health problem for Human Immu-
cine vendor (PMV) was noted to
Yakubu AM
nodeficiency virus (HIV) infected
be
the most risky practice leading
Department of Paediatrics,
population. Both infections share
to
HCV in children, with more
Muktar HM
same routes of transmission, and
than thrice the chances of HCV
Department of Haematology,
quite often co-exist, with dual
sero-positivity than in those who
Ahmadu Bello University Teaching
infections associated with recipro-
didn’t receive injections at PMV.
Hospital, Zaria, Nigeria.
cal and mutually more rapid pro-
Four mothers of the HIV-infected
Email: musa4all@gmail.com
gression than either infection
children were co-infected with
alone. Co-infection also adversely
HCV and none in the control
impacts on the course and man-
group. All 4 children of these
agement of both infections. This
dually infected mothers were also
study was carried out to document
co-infected. Controlling for other
the prevalence and determinants
factors, children of HIV infected
of
HCV sero-positivity in HIV-
mothers were more than twice as
infected children.
likely to have HCV antibody as
Methodology: A
total of
132 HIV-
children whose mothers were HIV
infected children attending the
negative (RR = 2.67). Similarly,
Paediatric Antiretroviral Clinic
HCV infected mothers have 12%
were recruited as subjects. An-
greater chance of transmitting
other 132 HIV negative children
HCV to their children than non-
matched for age and sex were
infected mothers and children de-
recruited as controls. Relevant
livered vaginally were 1.6 times
demographic data was taken from
more likely to have HCV antibody
each child. Blood samples were
than
those delivered via caesarean
also
obtained from each child and
section.
from their mothers when avail-
Conclusions: The
prevalence of
able, and assayed for the presence
anti-HCV in HIV-infected children
of
anti-HCV using a membrane-
is
significantly higher than that of
based immune-assay kit.
HIV uninfected peers. Factors
Results: The
sero-prevalence of
strongly associated with HCV sero
HCV antibodies was 9.8% among
-positivity identified are maternal
HIV-infected children and 3.0%
HIV and HCV infections, vaginal
among the controls. This was a
delivery and injections at patent
statistically significant difference
medicine vendor.
(p
= 0.042, Fisher exact). HCV
sero-postivity was more frequent
Key words: HCV;
HIV; children
in
children after 5 years of age in
Introduction
hepatocellular carcinoma (HCC).
2-3 HCV infection acts
as
an opportunistic disease in HIV-infected persons be-
Hepatitis C virus (HCV) and Human Immunodeficiency
cause of the increased incidence and accelerated natural
history in co-infected persons. HCV infection may also
4
virus (HIV) co-infection is a growing public health con-
cern. It has gained importance with decreasing AIDS-
1
impact the course and management of HIV disease, par-
related morbidity and mortality due to HIV treatment.
ticularly by increasing the risk of antiretroviral drug-
induced hepatotoxicity.
5-6
HCV/HIV co-infection is associated with higher HCV
viral load and a more rapid progression of HCV-related
It
is estimated that four to five million persons are co-
infected with HIV and HCV worldwide. According to
7
liver disease, leading to an increased risk of cirrhosisand

35
the World Health Organization (WHO), sub-Saharan
primary paediatrician managing the case.
Africa has the highest prevalence of both infections,
8
Approval of the Scientific and Ethical committee was
being home to almost two thirds (63%) of all persons
obtained before the commencement of the study.
infected with HIV and the majority of the 2.3 milion
children living with HIV worldwide and having esti-
9
Data Collection
mated 5.3% average prevalence for HCV.
10
Nigeria, with an overall HIV prevalence of 4.4%
11
in
Relevant data from all children enrolled for the study
2006and also appears to have a high incidence of HCV
was obtained and a detailed physical examination was
infection with estimated prevalence rates of up to 14%.
12
conducted at recruitment. Data obtained from history,
suggests a very high burden of co-infection with both
physical examination and laboratory results was re-
viruses and makes the country a potential source of an
corded into a specifically designed proforma.
emerging epidemic of HIV/HCV co-infection.
13
Prevalence rates of HIV/HCV co-infection depend on
Laboratory Methods
the mode of acquisation of both infections and the popu-
lation studied. Although both HIV and HCV share
Five millimetres of venous blood was taken each from
similar modes of transmission, the relative efficiency of
all patients and their mothers and centrifuged by the
transmission of the two viruses by different routes var-
investigator. Sera obtained were assayed for the pres-
ies. and mother to child transmission is the main route
14
ence of antibodies to hepatitis C virus (Anti-HCV). De-
of
acquiring both infections among children under the
tection of Anti-HCV was carried out using the HCV
age of 15 years.
15
One Step test kit for the qualitative detection of
antibodies to hepatitis C virus in serum or plasma.It is a
Only a few studies focussed on HIV/HCV coinfection
membrane-based immunoassay that is commercially
among the paediatric population even in most parts of
available.The kit has a relative sensitivity of 96.8% and
Africa and Nigeria where the potential for high disease-
specificity of 98.9%. Manufacturer's instructions were
burden exists.
16-19
Whether or not prevalence rates and
strictly followed to determine the serum samples that
other observations about hepatitis C virus and HIV co-
would be seropositive for HCV antibody.
infection in several adult populations can be projected to
children remains to be seen. This study therefore is
Data Analysis
aimed at determining the seroprevalence of HCV/HIV
co-infection in children aged 2 years to 15 years.
Data obtained from the study was analyzed using the
computer SPSS version 15.0.0. Results are presented in
figures, tables and graphs as appropriate. Differences
between proportions were evaluated by the Chi-square
Subjects and methods
test
with Yate’s correction applied as appropriate or
Study area
Fishers exact test was used where appropriate. A p-value
of
less than 0.05 was considered to be statistically sig-
The
study was conducted at the Paediatric Antiretroviral
nificant in comparative analyses. Relative risks with
(PARV) Clinic. The clinic is situated in a tertiary
95% confidence intervals were calculated.
referral hospital, and sees an average of 50 patients a
week from across the northern states.
Case Management of children
Study population and design
All children recruited for the study were routinely addi-
tionally investigated as appropriate based on their other
A
hospital-based prospective cross-sectional descriptive
presenting symptoms and signs to establish the existence
study of children between the ages of two years and fif-
or
otherwise of concomitant disease according to the
teen years attending the clinic was carried out. HIV
standard of care in the hospital. All the children re-
negative children, matched for age and sex, attending
cruited for the study were then managed accordingly
other paediatric specialist clinics, were recruited as con-
either in the Paediatric ARV Clinic, or the Paediatric
trols. Children were included in the study as cases if
Gastro-enterology, Hepatology and Nutrition clinic or in
aged between 2 and 15 years, have a HIV positivity and
any of the other paediatric units as appropriate.
are attending the PARV clinic. Inclusion in the study as
control was if they were aged between 2 and 15 years
and are HIV negative. Children were excluded from the
study if parents or caregivers declined consent for the
Results
study.
A
total of one hundred and thirty two HIV infected chil-
Ethical Consideration
dren who fulfilled the criteria for inclusion were pro-
spectively studied for presence of HCV antibody be-
Informed consent of each of the children’s parents or
tween November 2008 and August 2010 as study sub-
caregivers was obtained before recruitment into the
jects. Another 132 HIV negative children matched for
study. Pre-test and post-test counselling was done as
age and sex were studied as controls during the same
appropriate and test results were communicated to the
period.
36
Prevalence of antibody to HCV in study group and
Risk factors for anti-HCV positivity:
Controls
Table 3 shows risk factors of mode of delivery, early
Out of the 132 study subjects, 13 tested positive to HCV
breastfeeding status, and maternal anti-HCV, HIV status
antibody. This gives the prevalence of antibody to HCV
of
children with a positive anti-HCV in both study sub-
of
9.8% among the study subjects. Among the 132 con-
jects and the controls. Of the 13 study subjects with a
trols tested, 4 had antibody to HCV, giving a prevalence
positive anti-HCV, 12 (92.3%) were delivered vaginally
of
3.0% as shown in Table 1. The difference between
while 3 (75.0%) of the 4 controls with positive anti-
the two groups was statistically significant (p = 0.0142,
HCV were delivered vaginally. The relative risk of a
Fisher’s Exact test).
positive anti-HCV by vaginal delivery was 1.60 (95%
CI= 0.76 – 31.57) which was not statistically significant.
Table 1: Prevalence
of HCV
antibody in
study subjects
and
Eleven children with positive anti-HCV among the
controls
study subjects (84.6%) had been breastfed while among
Anti-
HIV
Controls
p-value
the controls, 1 (25.0%) of those with positive anti-HCV
HCV
(Fisher’s exact test)
had been breastfed as shown in table 3. The relative risk
Positive
13
(9.8)
4
(3.0)
was 1.18 (95% CI = 0.73- 6.10), which was also was not
Negative
119
(90.2)
128
(97.0)
0.042
a
statistically significant difference.
Total
132
(100.0)
132
(100.0)
Table 3 also shows HIV and HCV status of mothers of
Age prevalence
children with a positive anti-HCV among both study
subjects and controls. Not all mothers in both groups
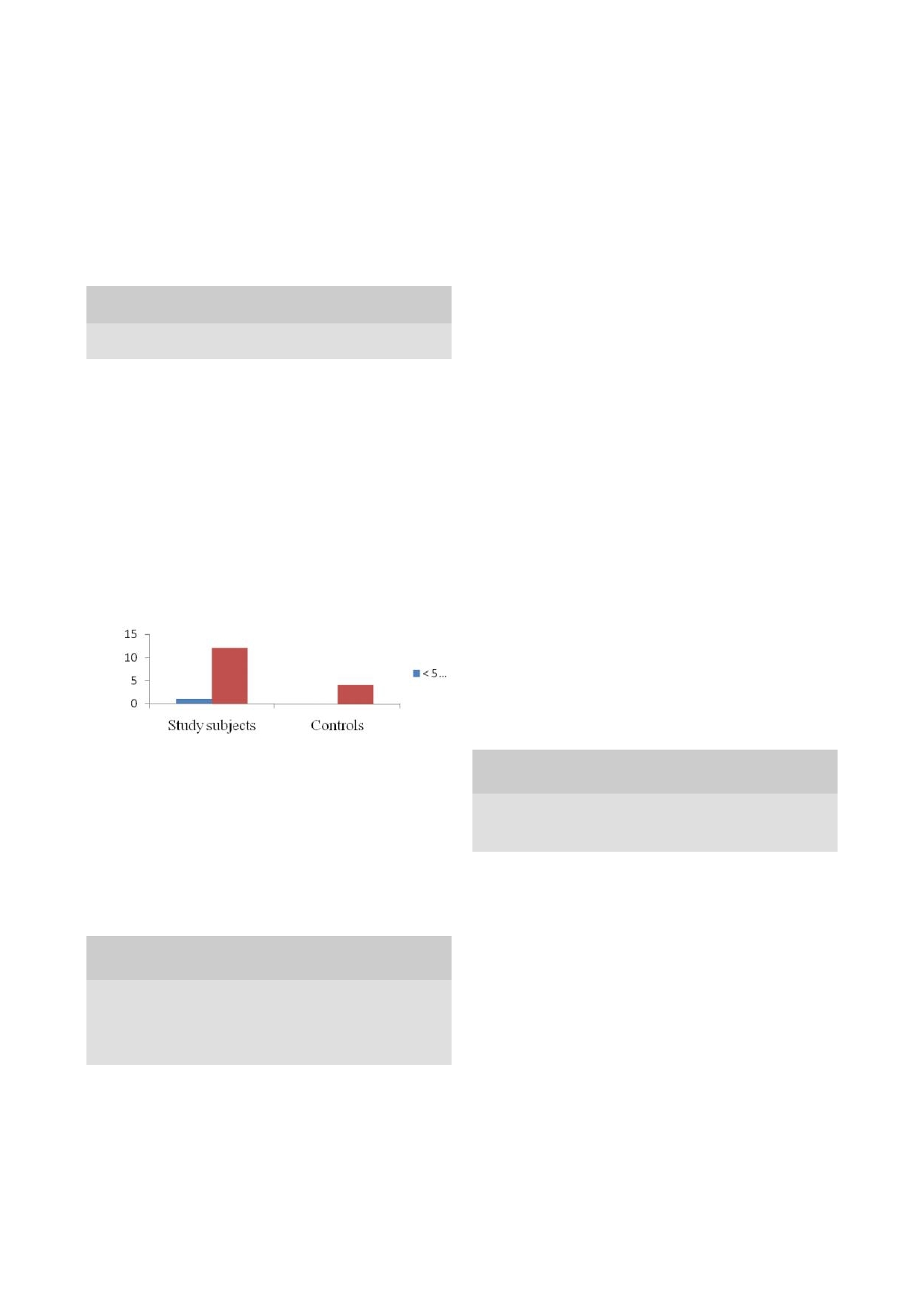
Fig 1 shows the prevalence of antibody to HCV by age
were available for testing. Four (44.4%) of the nine
among both the study subjects and the controls. Anti-
mothers of children in the study group also tested posi-
HCV positivity was detected more in children aged
tive for anti-HCV as against a mother (33.3%) out of 3
above five years in both study subjects and controls.
in
the control group. The relative risk for a positive anti-
This difference was statistically significant.
HCV was 1.12 (95% CI = 0.52 – 1.71). This however
(
χ2 = 1.000 with Yates correction, p = 0.00).
was not a statistically significant increased risk.
Similarly, 8(88.9%) of 9 mothers of children in the
Fig 1: Prevalence
of positive
anti- HCV
by age
among both
study subjects with positive anti-HCV were also HIV
the
study subjects and the controls
infected as against a mother out of the 3 (33.3) in the
control group. The relative risk was = 2.67 (95% CI =
0.83 – 33.18), which again was not statistically signifi-
cant.
Four mothers of the HIV-infected children were co
-infected with HCV and none in the control group. All 4
children of these dually infected mothers were also co-
infected.
Sex prevalence
Table 3: Maternally-associated risk
factors in
children with
positive anti-HCV among study subjects and controls
The distribution of antibody to HCV by gender is shown
Anti-HCV positive
in
table 2. Eight (6.1%) of the children among the study
Maternally-
Study
Controls,
Rela
95%
confidence
subjects who had positive antibody to HCV were males
associated
subjects,
n =
4
tive
interval
as
against 3(2.3%) among the controls. Five (3.8%)
risk
factors
n =
13
risk
among the study subjects with positive anti-HCV were
Mode of delivery:
females as against 1 (0.8%) among the controls. This
Vaginal
12
(92.3)
3
(75.0)
1.60
0.76 – 31.57
Caesarean
1
(7.7)
1(25.0)
0.63
0.03 – 1.32
difference was not statistically significant (p = 1.000,
Early infant feeding:
Fisher Exact test).
Ever breastfed
11
(84.6)
1
(25.0)
1.18
0.73 – 6.10
Never breastfed
2
(15.4)
3
(75.0)
0.85
0.16 – 1.37
Table 2: Distribution
of antibody
to HCV
by gender
in study
Maternal HIV and
n*
= 9
n*
= 3
subjects and controls
HCV
status:
Sex
Study
Controls, n (%)
Anti-HCV +ve
4
(44.4)
1
(33.3)
1.12
0.52 – 0.71
subjects, n
HIV
+ve
8
(88.9)
1
(33.3)
2.67
0.83 – 33.18
(%)
Anti-HCV
Anti-HCV
Anti-HCV
Anti-HCV
* n
is the number of mothers of children with positive anti-
positive,
negative,
positive,
negative,
HCV
available for assay
n =
13
n =
119
n =
4
n =
128
Male
8
(6.1)
73
(55.3)
3
(2.4)
80
(6-.6)
Other Risk factors
Female
5
(3.8)
46
(34.8)
1
(0.8)
48
(36.4)
Total
13
(9.8)
119
(90.2)
4
(3.0)
128
(97.0)
Other potential risk factors evaluated for positive HCV
antibody in both study subjects and controls including
(p
= 1.000, Fisher Exact test)
certain cosmetic, religious and cultural practices, unsafe
injections and exposure to blood or blood products as
shown in table 4.
Table 4 depicts the cosmetic, religious or cultural prac-

37
tices that may be potential risk factors for HCV infec-
ences may reflect differences in methods of HCV anti-
tion in children found to be anti-HCV positive among
body assay used and the differences in risk factors de-
study subjects and control groups.
pending on the age variations of populations stud-
ied.****
Of
the 13 study subjects with positive HCV antibody, 8
had tribal marks as against 2 out of 4 controls with posi-
It
was observed in this study that HCV antibody positiv-
tive HCV antibody. This gives a relative risk of a posi-
ity was more frequent after the age of five years. This
tive anti-HCV in study subjects and controls for tribal
was the case among both the study subjects and the Con-
marks, tattoos, uvulectomy, ear piercing, circumcision
trols, with no statistically significant differences be-
and transfusion and their corresponding 95% confidence
tween study subjects and Controls. There was however a
interval were 1.12 (95% CI = 0.68 – 1.98), 1.07 (95% CI
statistically significant difference between rates of HCV
=
0.45 – 1.47), 1.22 (95% CI = 0.63 – 1.64), 0.89, (95%
antibodies positivity and age less than or five years and
CI
= 0.52 – 2.55), 1.39 (95% CI = 0.62 – 2.41) and1.15
beyond. The increased rate of HCV sero-positivity be-
(95% CI = 0.55 – 1.55) respectively. All these were
yond five years found in this study may suggest the rela-
found not to be statistically significant as shown in table
tive importance of post-partum transmission due to
IV. However, 12 of 13 study subjects with positive HCV
greater cumulative opportunities for contact via continu-
antibody had received injections at patent medicine
ous or repeated exposure to risk factors as the child
stores as against a child among the control group. This
grows compared to peri-natal transmission. This is con-
was statistically significant, (RR = 3.69; 95% CI =1.03 -
trary to findings reported among children across eleven
44.55).
tertiary care centres in Nigeria where the median age
was 3.4 years, and elsewhere in which age was found
17
Table 4: Risk
factors for
positive HCV
antibody among
study
not to be significantly associated with anti-HCV sero-
subjects and controls
positivity.
16
The reasons for these differences however
Anti-HCV positive
are unclear. More epidemiologic data on HCV infection
Study
Con-
Rela-
Potential risk
in
HIV-infected children are required to make compari-
subjects,
trols,
tive risk
95%
Confi-
factors
son on the role of age as an independent risk factor. Sex
n =
13
n =
4
dence interval
was
not noted in this study to be of any significance in
Cosmetic, religious/cultural practices:
influencing the rates of HIV/HCV co-infection or HCV
Tribal marks
8
2
1.12
0.68 – 1.98
infection alone. Again this has been previously noted in
Tattoos
4
1
1.07
0.45 – 1.47
adult population. This is contrary to the report from
23
Uvulectomy
Ω
6
1
1.22
0.63 – 1.64
Tanzania
16
Ear
piercing
+
4
2
0.89
0.52 – 2.55
among HIV-infected children in which the
Circumcision
*
5
2
1.39
0.62 – 2.41
prevalence of HCV antibody positivity was significantly
Use of blood/blood products:
higher among girls than boys. On the other hand, the
Transfusion
5
1
1.15
0.55 – 1.55
study across 11 care centres in Nigeria found 76% of
HCV co-infected children to be males. The reason for
17
Unsafe use of sharps:
Injection at
12
1
3.69
1.03 – 44.55
these differences is not clear.
PMV
One aim of this study was to document risk factors of
+
Ear piercing was seen only in girls * Circumcision was seen only
among boys
transmission. The various potential risk factors of trans-
PMV
= Patent medicine vendor
Ω
A
cultural practice done by tradi
mission of HCV in both HIV infected subjects and con-
tional barber
trols were therefore also explored. The possible role of
mode of delivery as a risk factor was examined. Obser-
vations in this study showed that children who were
Discussion
vaginally delivery were 1.6 times more likely to have
positive HCV antibodies than children delivered via
This study has shown the presence of HCV antibodies in
caesarean section. This however was not statistically
HIV infected children aged 2 to 15 years as well as in
significant. There is a similar report of no statistically
age and sex-matched controls. The prevalence of HCV
significant difference between different modes of deliv-
ery and rates of HCV transmission or infection. The
15
antibodies in HIV infected children aged 2 to 15 years
was 9.8%. The prevalence of HCV antibodies in HIV
present study was not able to further segregate delivery
negative children aged 2 to 15 years was 3%. This dif-
methods into normal vaginal or instrumental and as-
ference in the prevalence rates between the study sub-
sisted vaginal deliveries on one hand, and elective or
jects and controls is statistically significant, and suggests
emergency caesarean section on the other hand because
an
increased rate of HCV sero-positivity among HIV
of
inconclusive information from caregivers as to what
infected children. This has been previously documented
type of vaginal delivery or section was used in some
by
other workers in Tanzania
16
and
also across Africa
cases. There is nevertheless a case of a clinically in-
among different adult populations.
20-24
The 9.8% HIV/
creased risk of HCV antibody positivity when delivered
HCV co-infection rate found in this study is far lower
via vaginal route over caesarean section.
than the 20.2% rate reported in Jos among adult popula-
tion, but much higher than rates of 0.02% - 3.3% re-
25
Breastfeeding was another potential risk factor explored
ported by other workers in paediatric population
17
and
in
this study. It was observed that breastfed children in
elsewhere among adult populations.
26-27
These differ-
the study were 1.18 times as likely to have a positive

38
HCV antibody as their non-breastfed peers. Again, this
study. Five of the 13 children (38.5%) among the study
was not of statistical significance. The marginal increase
subjects with a positive HCV antibody had a history of
in
risk was in keeping with other studies that showed
previous blood transfusion as against one of four (25%)
that transmission via breast milk was not a significant
among the controls with positive HCV antibodies. This
mode of transmission in spite of detection of HCV RNA
was not a statistically significant difference. The finding
in
the breast milk of viraemic mothers.
15,
20
It
was sug-
in
this study was not entirely unexpected as transfusion
gested that acquisition of HCV by children through
of
blood or blood products carried out in standard health
breastfeeding will be dependent on the viral load in the
facilities offering transfusion services such as this centre
breast milk, which is usually said to be highest soon
usually screen the blood or blood component for HCV.
after delivery. It was not possible to substantiate this in
28
Significant HCV nosocomial transmission through
the present study because maternal HCV viral load in
transfusion of blood or its components would only occur
blood or breast milk was not determined.
in
settings with absence of blood screening services.
That was not the setting in this environment.
This study however determined the maternal HCV anti-
Certain cosmetic, cultural or religious practices were
body status and how it relates to HCV antibody positiv-
identified in the present study to marginally raise the
ity
in both the study subjects and the controls. It was
risk
of positive HCV antibodies. These included tribal
noted that HCV seropositive mothers with HIV infection
marks and tattoos, which increased the chances of trans-
had
a 12% increased chance of having children with
mission by 1.12 and 1.07 times more than in those with-
HCV antibody positivity than HCV sero-negative moth-
out these procedures respectively. These figures how-
ers. Although a mother with HCV infection could trans-
ever did not reach statistical significance. Other risky
mit it vertically to her children, this however does not
practices of note in this study were uvulectomy and cir-
conclusively prove route of transmission.
cumcision, which increased the probability of HCV anti-
body positivity by 1.22 and 1.39 times respectively more
This study was not designed to determine the route of
than in children who did not have them. Again, these
HCV transmission for co-infected children. Further tests
were not statistically significant.
would be required to confirm if transmission was mother
-to- child when mother-child pair is found to have HCV
All these practices, especially tribal marks, tattoos and
infection, since both may have acquired the HCV infec-
uvulectomy, and to a less extent circumcision, in our
tion from the same source. It was not possible from the
environment are carried out by traditional barbers, often
design of the present study therefore to speculate on
using the same blade for multiple subjects with little or
possible vertical transmission of HCV infection among
no
sterilization before re-use. This setting would highly
favour HCV transmission.
10
study subjects and controls.
This study has demon-
strated weak associations of these very common prac-
Maternal HIV infection was observed to enhance HCV
tices in our environment with HCV antibody positivity,
antibody positivity in children in this study. Eighty eight
which because of their widespread practice in the com-
percent (8/9) of mothers of children with positive HCV
munity cannot be overlooked as potentially risky proce-
antibodies available for assay were HIV infected among
dures.
the cases as against one of three (33.3%) corresponding
mothers among the controls. Children whose mothers
Surprisingly, it is noteworthy that this study found no
were HIV infected were found to be more than twice as
association between ear piercing and HCV antibody
likely to have HCV antibody positivity as children
positivity. It was expected that this very common cos-
whose mothers were HIV negative. This is in confor-
metic and cultural practice in the community would also
mity with reports that vertical transmission rates for
be
potentially risky considering that non-professionals
HCV were 8 to 40% higher for women who were also
commonly perform it. In this study however, it was ob-
HIV infected.
15
served that children who had their ear pierced had 0.89
times the probability of HCV antibody positivity than
The role of some other potential risk factors for trans-
girls who did not have ear piercing done. Perhaps a
mission was also explored. Results from this study sug-
plausible reason for this relative decreased risk may be
gested that unsafe therapeutic injection practice by pat-
because of the less likelihood of re-use of needle used
ent medicine vendors was a very significant risk factor
for the procedure than in other cultural procedures such
for HCV transmission in this environment. Twelve of
as
circumcision or uvulectomy.
thirteen (92.3%) children with positive HCV antibodies
Overall, this study has demonstrated the prevalence of
among the study subjects were noted to have had a his-
HCV antibody in HIV infected children to be statisti-
tory of injection at patent medicine shops as against a
cally different from that in HIV negative children. This
quarter of children with positive HCV antibodies among
underscores the importance of routine screening of all
the controls. This was a statistically significant differ-
HIV-infected children for HCV infection, to avail them
ence between the groups. This was much higher than the
with prompt and adequate treatment. The study has also
39% of co-infected patients reported in one cohort of
documented some possible risk factors for HCV/HIV co
having had a history of needle injection at patent medi-
-infection in these children and highlights the need to
cine stores.
23
provide safer injection practices especially to HIV in-
Blood transfusion was yet another risk factor usually
fected children through a combination of education, leg-
associated with HCV infection explored in the present
islation and regulation of patent medicine vendors.

39
Conflict of interest: None
Funding: None
References
1.
Rockstroh JK and Spengler U.
10.
WHO. Hepatitis C - global preva-
20.
Muktar HM, Alkali CN, Jones EM.
HIV
and hepatitis C virus co-
lence (update) Wkly Epidemiol
Hepatitis B and C co-infections in
infection. Lancet
Infect Dis
2004;
Rec.1999;74:425-7.
HIV/AIDS patients attending ARV
4: 437-44
11.
Nigeria Federal Ministry of
center ABUTH, Zaria, Nigeria.
2.
Bica I, Mcgovern B, Dhar R,
Health. Technical Report on 2005
HMR J 2006;4:39-45.
Stone D, McGowan K, Scheib R et
National HIV/Syphilis Sentinel
21.
Ayele W, Nokes DJ, Abebe A,
al. Increasing
mortality due
to end
Survey among pregnant women
Messele T, Dejene A, Enquselassie
-stage liver disease in patients with
attending antenatal clinics in Nige-
F
et al. Higher prevalence of anti-
human immunodeficiency virus
ria. Abuja. Nigeria: FMOH;2005.
HCV
antibodies among HIV-
infection. Clin.
Infect. Dis.
2001;
12.
Madhava V, Burgess C, Drucker
positive compared to HIV-negative
32:492 – 7
E.
Epidemiology of chronic hepati-
inhabitants of Addis Ababa,
3.
Benhamou Y, Bochet M, Di
tis
C virus infection in sub-Saharan
Ethiopia. J
Med Virol2002;68:12-7
Martino V, Charlotte F, Azira F,
Africa. Lancet
Infect Dis
2002;2:
22.
Agwale SM, Tanimoto L, Womack
Coutellier A et al. Liver fibrosis
293-302.
C,
Odama L, Leung K, Duey D et
progression in human immunode-
13.
Mboto CI, Davies A, Fielder M,
al.
Prevalence of HCV co-infection
ficiency virus and hepatitis C virus
Jewell AP. Human
in
HIV-infected individuals in
coinfected patients. The Multiviric
immunodeficiency virus and
Nigeria and characterization of
Group. Hepatology
1999;30:1054
hepatitis C co-infection in sub-
HCV
genotypes. J
Clin Virol
–
1058.
Saharan West Africa. Br
J Biomed
2004;31:S3-6.
4.
Sulkowski MS, Mast EE, Seeff
Sci. 2006;63:29-37.
23.
Inyama PU, Uneke CJ, Anyanwu
LB,
Thomas DL. Hepatitis C Vi-
14.
Koziel MJ, Peters MG.Viral Hepa-
GI,
Njoku OM, Idoko JH, Idoko
rus
Infection as an Opportunistic
titis in HIV Infection. N
Engl J
JA.
Prevalence of antibodies to
Disease in Persons Infected with
Med 2007:356;1445-54.
Hepatitis C virus among Nigerian
Human Immunodeficiency Virus.
15.
Nigro G, D’Orio F, Catania S,
patients with HIV infection.
Online
Clin Infect Dis 2000;30:S77-84
Badolato MC, Livadiotti S, Ber-
J Health Allied Scs.2005;2:2
5.
Greub G, Ledergerber B, Battegay
nadi S et al. Mother to infant trans-
24.
Forbi JC, Gabadi S, Alabi R, Ipere-
M,
Grob P, Perrin L, Furrer H, et
mission of coinfection by human
polu HO, Pam CR, Entonu PE,
al.Clinical progression, survival,
immunodeficiency virus and hepa-
Agwale SM. The role of triple
and
immune recovery during anti-
titis C virus: prevalence and clini-
infection with hepatitis B virus,
retroviral therapyin patients with
cal
manifestations. Arch
Virol
hepatitis C virus, and human im-
HIV-1 and hepatitis C virus co-
1997;142:453-457.
munodeficiency virus (HIV) type-1
infection: the Swiss HIV Co-
16.
Telatela SP, Matee MI, Munubhi
on
CD4 + lymphocyte levels in the
hortStudy. Lancet.
2000;356:1800
EK.
Seroprevalence of hepatitis B
highly HIV infected population of
-5.
and
C viral co-infections among
North-Central Nigeria. Mem
Inst
6.
Sulkowski M, Thomas D, Mehta
children infected with human im-
Oswaldo Cruz. 2007;102:535-537.
S,
Chaisson R, Moore R. Hepato-
munodeficiency virus attending the
25.
Gwamzi N, Hawkins C, Meloni S,
toxicity associated with nevirapine
paediatric HIV care and treatment
Muazu M, Badung B, et al. Impact
or
efavirenz-containing antiretro-
center at Muhimbili National Hos-
of
Hepatitis C Virus on HIV-
viral therapy: role of hepatitis C
pital in Dar-es-Salam, Tanzania.
infected individuals in Nigeria.
and
B infections. Hepatology
BMC
Public Health 2007;7;338.
Abstact 921. 14th Conference on
2002;35:182-189.
17.
Rawizza H, Ochigbo S, Chang C,
Retroviruses and Opportunistic
7.
Tossing G. Management of
Melonil M, Oguche S, Osinusil K,
Infections Los Angeles, California,
chronic hepatitis C in HIV-
etal . Prevalence
of Hepatitis
Co-
February 2007.
coinfected patients – results from
infection Among HIV-Infected
26.
Ejele E, Osaro E, Chijioke AN.
the
First International Workshop
Nigerian Children in the Harvard
The
Prevalence of Hepatitis C
on
HIV and Hepatitis Co-
PEPFAR ART Program. Confer-
Antibodies in Patients With HIV
Infection, December 2-4, 2004,
ence on Retroviruses and Oppor-
Infection In The Niger Delta Of
tunistic Infections; February 16 -
th
Amsterdam, Netherlands. Eur
J
Nigeria Osekhuemen. Highland
19
; San Francisco CA; 2010.
th
Med Res 2005;10:43-5.
Med Res J. 2005;3:11-17.
8.
Gisselquist D, Perrin L, Minkin
18.
Resti M, Azzari C, Bortolotti F.
27.
Inyama PU, Uneke CJ, Anyanwu
SF.
Parallel and overlapping HIV
Hepatitis C virus infection in chil-
GI,
Njoku OM, Idoko JH, Idoko
and
bloodborne hepatitis epidem-
dren coinfected with HIV: epide-
JA.
Prevalence of antibodies to
ics
in Africa. Int
J STD
AIDS
miology and management. Pediatr
Hepatitis C virus among Nigerian
2004;15:145 – 152.
Drugs 2002;4:571-80.
patients with HIV infection.
Online
9.
UNAIDS/WHO The Joint United
19.
Schuval S, Van Dyke RB, Lindsey
J Health Allied Scs.2005;2:2
Nations Programme on HIV/
JC,
Palumbo P, Mofenson LM,
28.
Rousseau CM, Nduati RW,
AIDS/World Health Organization.
Oleske JM et al. Hepatitis C Preva-
Richardson BA, Steele MS, John-
AIDS epidemic update. UNAIDS/
lence in Children with Perinatal
Stewart GC, Mboi-Ngacha DA et
WHO. [Internet]. 2006. [cited
Human Immunodeficiency Virus
al.
Longitudinal analysis of human
2007 Sep 3]. Available from:
Infection Enrolled in a long-term
immunodeficiency virus type 1
http://www.who.int/hiv/
Follow-up Protocol. Arch
Pediatr
RNA
in breast milk and its
mediacen-
Adolesc Med2004;158:1007-1013 .
relationship to infant infection and
tre/2006_EpiUpdate_en.pdf
maternal disease. J
Infect Dis
2003;187:741-47.